How to Lower Morning Blood Sugar If You Have Diabetes: 4 Tips

Keeping tight control of morning blood sugar levels for people with diabetes means one step closer to normal A1C and general well-being. In the article, we offer some tips to help you lower your sugar when you wake up.
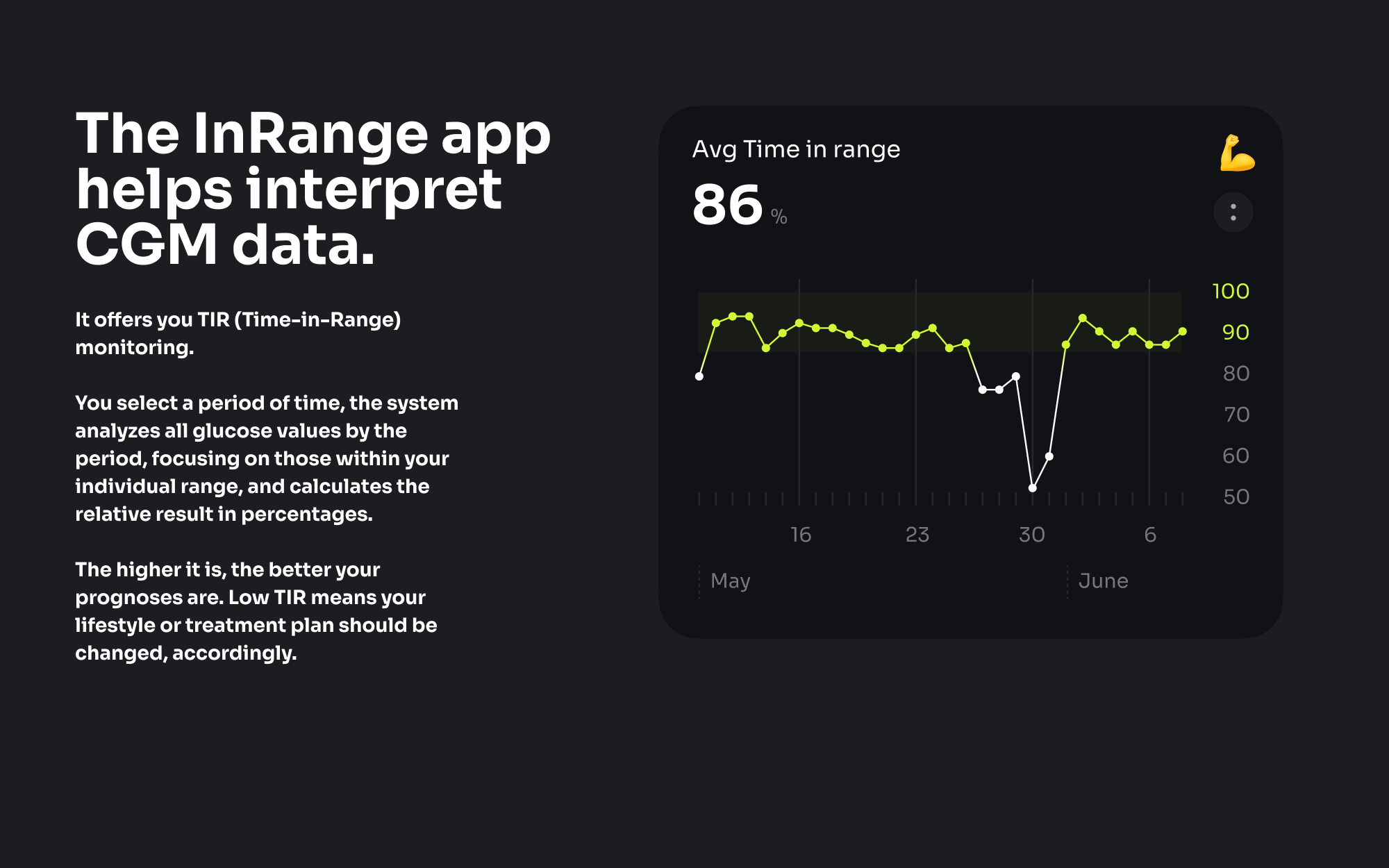
While developing the InRange app, we aimed to simplify managing diabetes by monitoring the long-term CGM (Continuous Glucose Monitoring) data changes. Thanks to the app’s graphs, you can analyze it to understand your individual causes of high glucose levels at any time of day and night.

Tip 1. Use a CGM device to see your patterns and lower sugar
With a CGM device, you can identify patterns in your glucose levels and make comprehensive decisions on how to best manage diabetes. It can provide insight into how different lifestyle choices affect blood sugar levels, such as food intake, exercise, sleep duration, and stress.
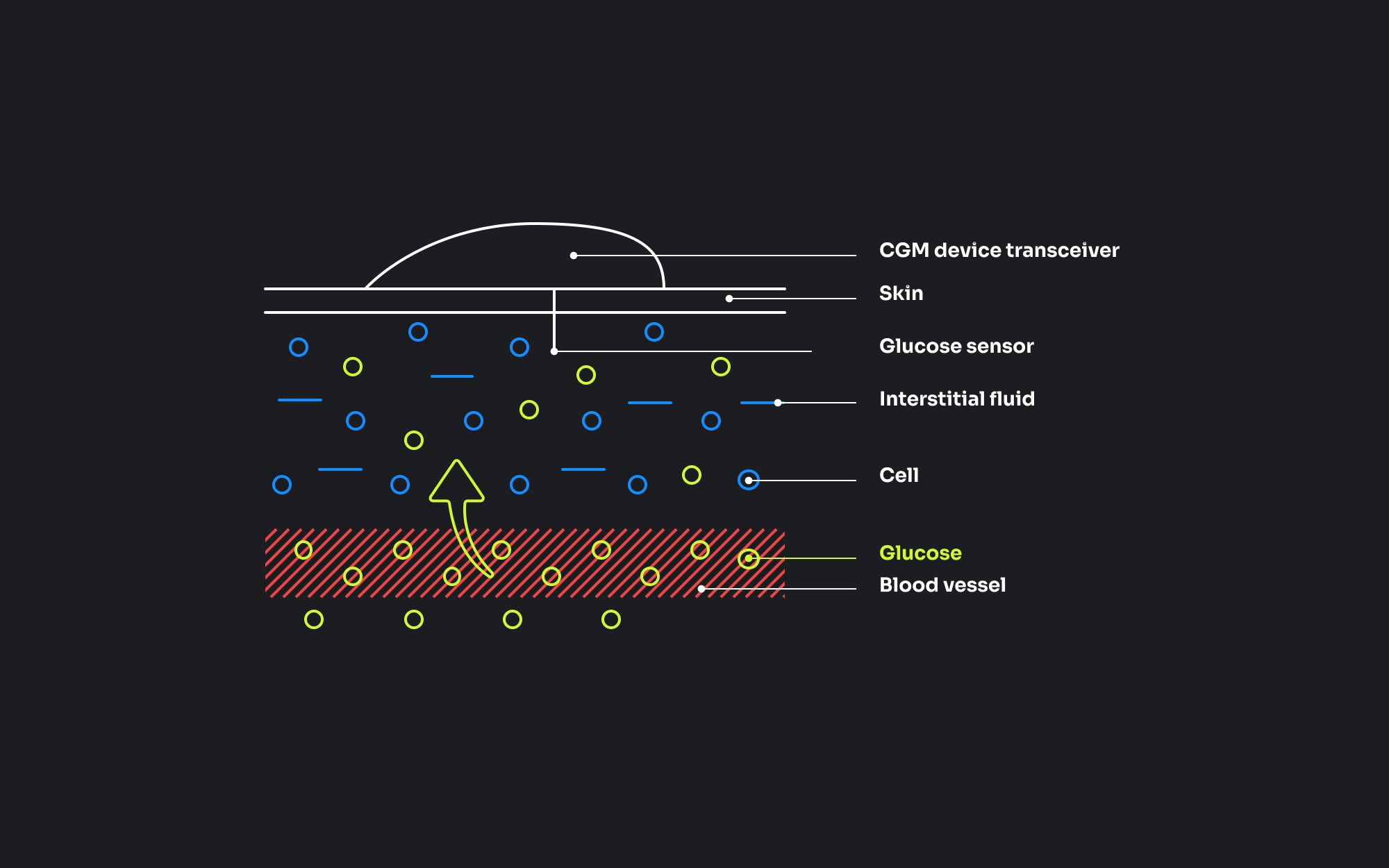
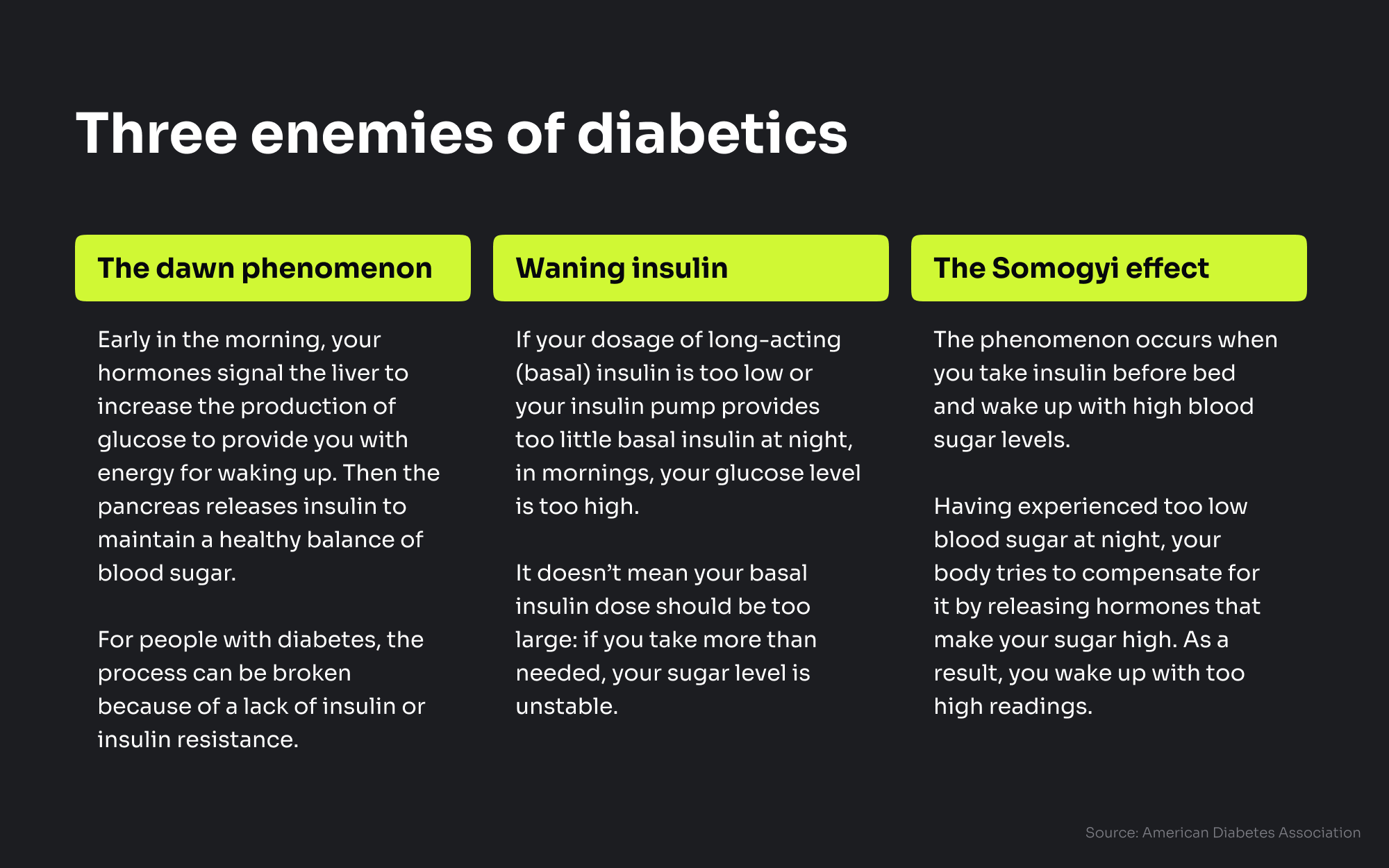
By monitoring your glucose before you go to bed, in the middle of the night, and when you wake up, you’ll find out at what time it is increased most often.
After you have noticed your personal trend, you can understand what changes are needed to lower morning glucose.
- For those who have high levels of glucose before going to bed, the thing is nutrition and medication / treatment plan.
- If your glucose level is normal at bedtime, the reason for increased morning sugar is medication / treatment plan.
Once you’ve found out your patterns, it’s time to discuss the further actions with your doctor.
Tip 2. Find your balance of insulin and glucose at bedtime
Normal glucose levels in the morning start with careful dietary choices for evenings. Avoid having large dinners or snacks just before you go to bed. Otherwise, your glucose level stays high for the whole night, while insulin is too low.
Evening carbohydrates are a bad idea. The sooner your bedtime is, the less carbs you should take because 100% of them are converted to glucose, and it can cause high fasting glucose

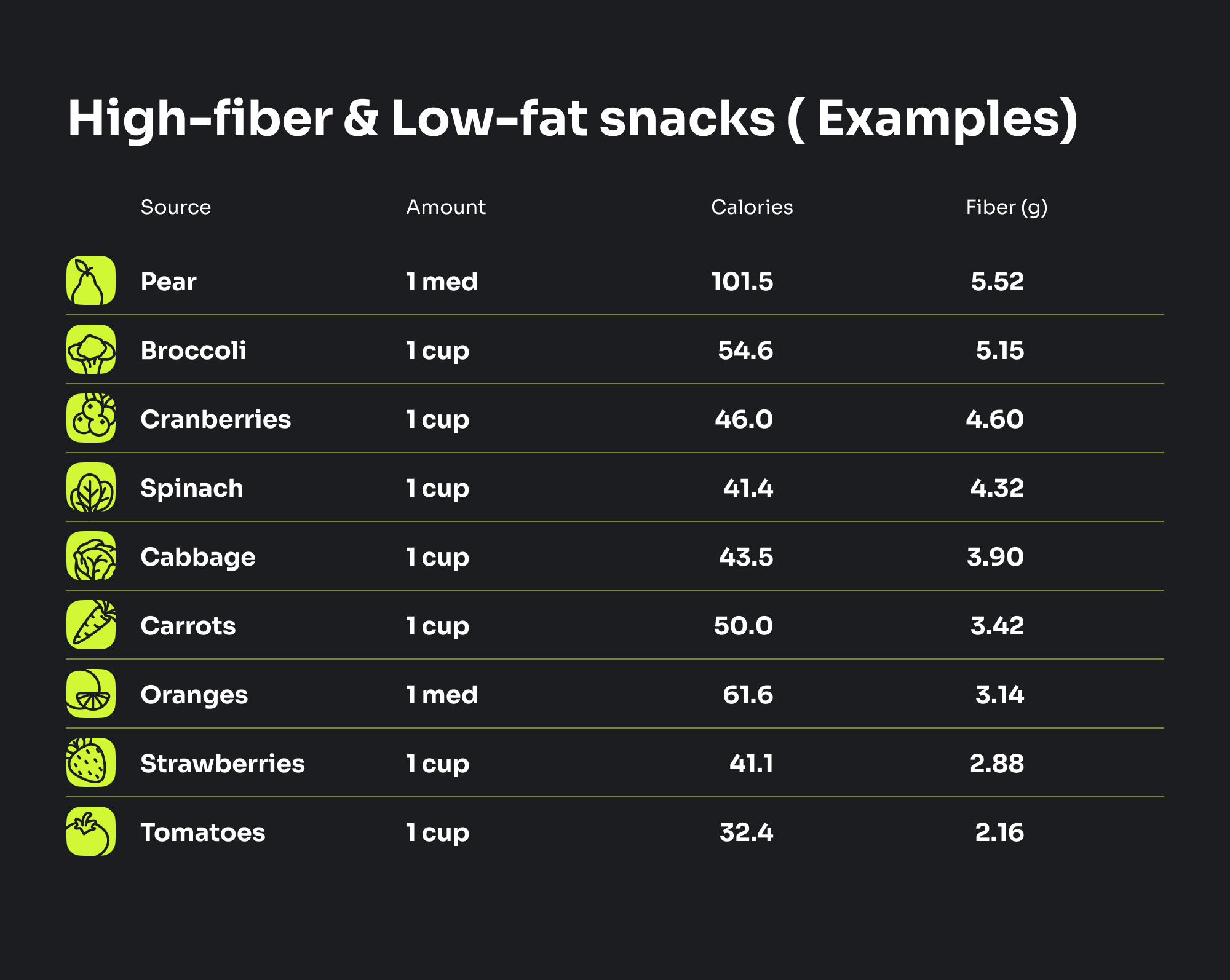
According to the American Diabetes Association, 45–60 g of carbs per meal and 15–20 g per snack is recommended for people with diabetes. The exact amount can be changed depending on your weight, target blood sugar levels, activity, and other factors.
What to eat in the evening instead? High-fiber and low-fat snacks can satisfy your hunger, and they won’t have a negative impact on glucose levels at night and in the morning.
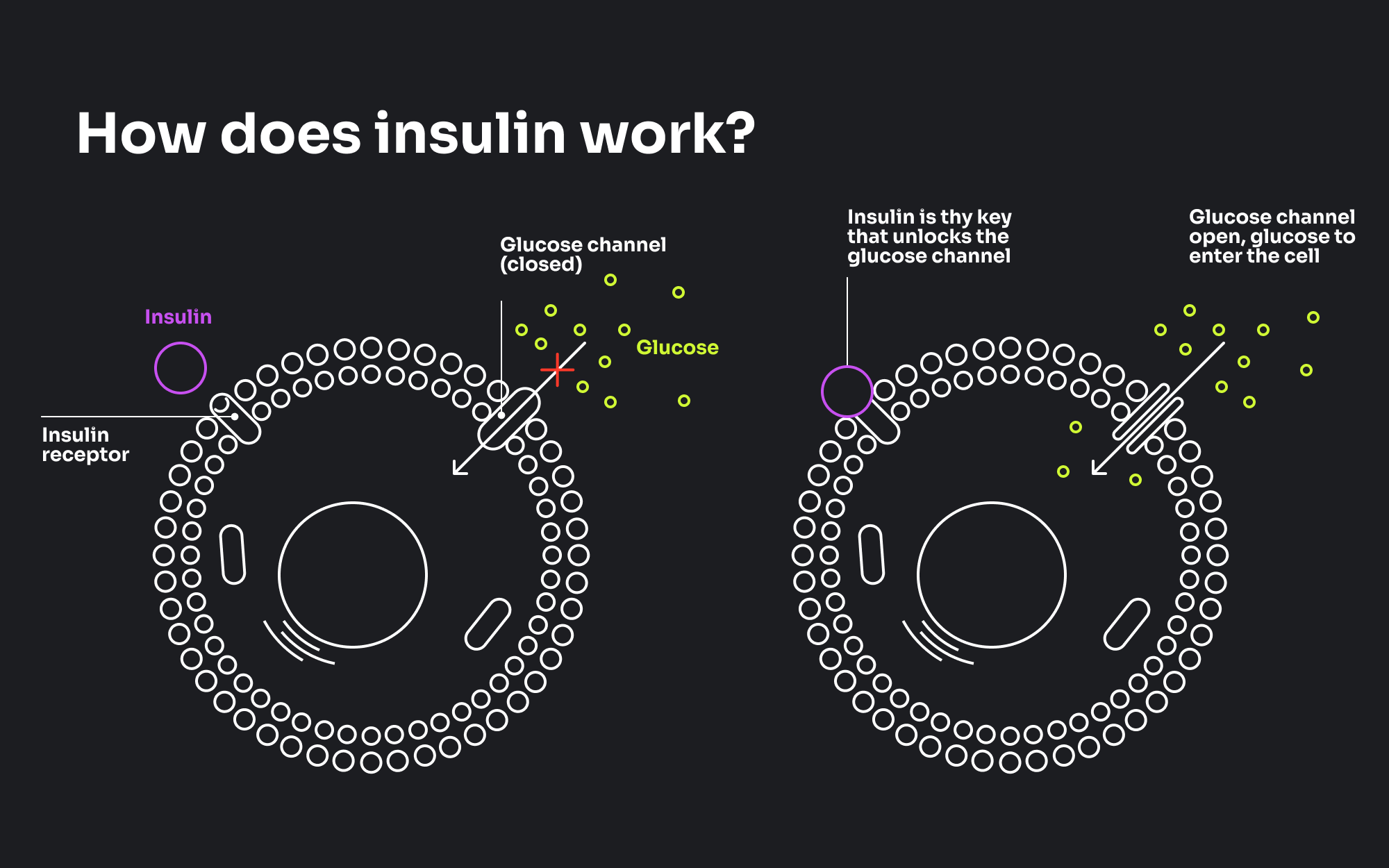
Be sure that you get enough insulin to compensate for the amount of carbs taken throughout the day for type 1 diabetes, or medicines to treat insulin resistance for type 2 diabetes.
Tip 3. Add middle intensity workout for 30+ minutes a day regularly
Listen to your body and take regular breaks when engaging in a middle intensity workout. This will help ensure that you are exercising appropriately for your fitness level and health factors. Examples of middle intensity workouts include
- brisk walking
- jogging
- cycling
- dancing
- swimming
Aerobic exercises such as these can help to improve blood sugar control, reduce body fat, and increase insulin sensitivity.
In addition to aerobic exercises, strength training is also beneficial for diabetics as it can help build muscle mass and improve glucose metabolism. However, these exercises should be chosen and performed with caution, as they can have a greater effect on glucose levels than aerobic activities and put additional strain on the body. For diabetics, too extreme lowering of glucose can be dangerous because of hypoglycemia risks.
Besides aerobic and strength training, you shouldn’t forget about stretching and making 10,000 steps a day at least to feel well and reduce the risks of diabetes complications. Be careful with evening training to avoid hypoglycemia at night. If you do them, the practices shouldn’t be intensive or long. In addition, monitoring your glucose before and after exercises is important to have a strong control over it.
Tip 4. Focus on long-term goals to stay in range most of the time
Once you’ve found out how to lower morning blood sugar and succeed in it, it’s time to get more control over your diabetes throughout the day and night.
According to recent research, poor control of diabetes results in 8 years of life lost for T1D and 2 years for T2D. So, the more time you are in range, the better you can manage your condition and the less damage your organs get.
The InRange App is developed to help diabetics control their long-term changes. Focusing on them and correcting your habits or treatment plan, you can get up to 8 years of life back.
How does it work? With the app graphs, you can easily monitor CGM data changes by days, weeks, and months to see your personal patterns. Based on the data, you and your healthcare provider can make up the best treatment plan.
To sum up
High morning blood sugar can be caused by a number of factors including what you ate the night before, whether you got a good night’s sleep, your hormones, and physical activity levels.
While choosing a way of controlling your health, remember that the solution is always individual and use technologies that can be easily integrated into your daily routine, providing reliability and accuracy.
